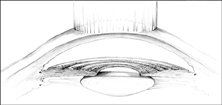
Excimer Laser Photorefractive Keratectomy (PRK)
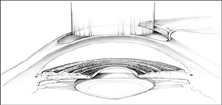
Excimer Laser In SituKeratomileusis (LASIK)
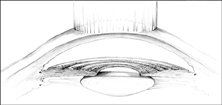 Excimer Laser Photorefractive Keratectomy (PRK)
|
Refractive surgery is the modification of the optical components of the eye to reduce or eliminate an individual's dependence on glasses or contact lenses. The number of refractive procedures performed has surged in recent years due to strong patient demand and increased physician acceptance. Despite the popularity of refractive surgery, many questions remain regarding the visual function of patients after surgery. Patient complaints after refractive surgery include impaired night vision, glare, halos, and blurred vision. Some patients may experience these vision problems despite 20/20 visual acuity. Our goal is to determine whether patients who have undergone refractive surgery have impaired visual function which could impact automobile driving ability, and if these effects can be quantified and monitored using a computer-based driving simulator.
The overall objective of this research is to develop a safe and objective method for assessing visual function in this essential daily living activity. Successful validation of this approach will provide a new paradigm for systematic analysis and monitoring of the functional visual effects of refractive surgery. These methods may also be useful in assessing the functional impact of other medical conditions and procedures.

This research is being done in conjunction with the UW Dept. of Ophthomology Refractive Surgery Center. A high-end computerized driving simulator will be used to measure driving performance under daytime, night and fog conditions. The RealDrive driving simulator, under the direction of the Human Interface Technology Laboratory at the University of Washington, offers a fully immersive simulated driving experience. Refractive surgery patients from the University of Washington Medical Center's Refractive Surgery Clinic will be tested three times on the driving simulator: before surgery, three months post-operatively, and one year after surgery. Each participant will drive through a practice course followed by a standard course in each of the three lighting conditions. The total simulation time for each patient session will be limited to 25-30 minutes, to minimize the risk of any adverse effects of the simulation.
Each subject's driving performance will be assessed according to the following criteria: simulator accidents, road position and lane keeping, driving speeds, and hazard detection. Pre-operative and post-operative driving performance measures will be compared using appropriate within-subjects statistics. Self-report surveys will also be administered to each subject, with a focus on validating the lighting and driving condition models used in the simulation.