|
Virtual Reality Exposure therapy
for Post Traumatic Stress Disorder (click here).
Virtual Reality Exposure therapy for Spider
phobia (click here).
Magnet-friend fMRI brain scans studing changes
in pain-related brain activity associated with virtual reality analgesia
(click here).
Water-friendly virtual
reality helmet for treating burn patients who are sitting in a tub of water
during wound care (click here).
"Virtual Reality Therapy" article published in the Aug 2004 issue
of Scientific American Magazine
(see also www.sciam.com)
To see a 1 min digital video clip interview of a
6 year old burn patient after virtual reality…click
here
or just keep scrolling down to see our website on using virtual reality to
treat pain in burn patients.
Click here to learn
about Pain, Mind and Movement - A Satellite Symposium of the 11th World
Congress on Pain, 17 – 19 August 2005, Cairns International Hotel, Cairns,
Australia at the Great Barrier Reef in Australia for a hands-on immersive
VR demonstration of SnowWorld, and a presentation by Hunter about our
teams empirical studies of VR analgesia for severe burn pain. http://www.venuemarketing.com.au/pain.html
above image
Copyright © Miss Howie Chambers.
All images on this
webpage are copyrighted.
Harborview research
nurse Gretchen Carrougher RN (left) and Verna Cain, RN (right) removing staples from a skin
graft of a burn patient in virtual reality.
How to donate
Introduction: The University of Washington
Harborview Burn Center, directed by Dr. Nicole Gibran, is a regional burn
center. Patients with severe burns from 5 surrounding states are sent to
Harborview for special care. Harborview has pioneered a number of advanced
treatments (e.g., early skin grafting). As a result of advances here and
elsewhere, the chances of surviving a bad burn, and quality of living for
survivors has improved dramatically over the past 20 years.
Unfortunately, the amount of pain and
suffering experienced by patients during woundcare remains a worldwide
problem for burn victims as well as a number of other patient
populations.
As can be seen from the figure below,
when patients are resting (most of the time), opioids (morphine and
morphine-related chemicals) are adequate for controlling their burn pain (few
patients are in the red zone).
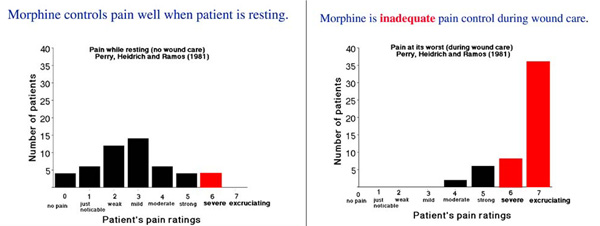
In sharp contrast, during wound care
such as daily bandage changes, wound cleaning, staple removals etc., opioids
are not enough, not even close. As shown in the figure below, over 86% of the
burn patients reported having severe to excruciating pain during wound care
(shown in red), even when standard levels of opioids were used. The pain
management techniques in use are not good enough. Patients are suffering, a
fact particularly disturbing when the patients are children.
In 1996, Hunter Hoffman and David
Patterson co-originated the new technique of using immersive VR for pain
control. Hunter is a VR
researcher from the U.W. Human Interface Technology Laboratory with a
background in human cognition and attention. Since 1993 he has been exploring
ways to increase the illusion of going inside virtual worlds (presence), how
VR affects allocation of attentional resources, and therapeutic applications
of VR. Professor
David R. Patterson studies psychological techniques (e.g., hypnosis) for
reducing severe acute burn pain of patients at Harborview Burn Center in
Seattle. Dave is head of the Division of Psychology of the U.W. Dept of
Rehabilitation Medicine. He is a recipient of the Milton H. Erickson
Award for Scientific Contributions to Hypnosis, and has a grant from NIH to
study VR burn pain control. Our interdisciplinary research team is using VR
adjunctively, IN ADDITION TO TRADITIONAL opioids. This team includes
Sam Sharar, MD., Gretchen Carrougher, RN, MN and Mark Jensen, Ph.D.

David Patterson
The first virtual world used was SpiderWorld.
Spiderworld was originally designed to treat spider phobics,
but has also proved quite distracting for burn patients.
With funding from NIH, the Paul G. Allen Family Foundations,
the William Randolph Hearst
Burn Center in New York, and local donors, we are now developing several new
virtual environments specifically designed for treating pain (e.g.,
especially attention-grabbing virtual environments designed to minimize or
avoid simulator sickness).
SnowWorld has been developed in a
collaboration between Hunter Hoffman, Multigen-Paradigm
Inc (Jeff Bellinghausen, and Chuck Walter), and SimWright Inc. (Brian
Stewart), Howard Abrams, with support from the Paul G. Allen Foundation (Paul
Allen and Bill Gates co-founded Microsoft).
In SnowWorld, patients fly through an
icy canyon with a river and frigid waterfall. Patients shoot snowballs at
snowmen and igloos (with animated impacts). Since patients often report
re-living their original burn experience during wound care, SnowWorld was
designed to help put out the fire.

A snapshot of SnowWorld,
image by Stephen Dagadakis, copyright Hunter Hoffman, U.W.
Our logic for why VR will reduce pain is as follows. Pain perception has a
strong psychological component. The same incoming pain signal can be
interpreted as painful or not, depending on what the patient is thinking.
Pain requires conscious attention. The essence of VR is the illusion users
have of going inside the computer-generated environment. Being drawn into
another world drains a lot of attentional resources, leaving less attention
available to process pain signals. Conscious attention is like a spotlight.
Usually it is focussed on the pain and woundcare. We are luring that
spotlight into the virtual world. Rather than having pain as the focus of
their attention, for many patients in VR, the wound care becomes more of an
annoyance, distracting them from their primary goal of exploring the virtual
world.
In our preliminary case study (Hoffman, Doctor, Patterson, Carrougher and Furness, 2000),
two patients with severe burns went into SpiderWorld. They saw a virtual
kitchen complete with kitchen countertops, a window with a partly cloudy sky,
as well as 3-D cabinets, and doors that could be opened and shut. Patients
could pick up a teapot, plate, toaster, plant, or frying pan by inserting
their cyberhand into the virtual object, and clicking a grasp button on their
3-D mouse. Each patient also physically picked up a virtual wiggly-legged
spider possessing solidity and weight, using a mixed-reality force feedback
technique developed by one of our team members. Patient 1 had 5 staples
removed from a burn skin graft while playing Nintendo, and six staples
removed from the same skin graft while in VR. He reported dramatic reductions
in pain during VR.
Patient 2 was perhaps a bigger
challenge. He had a severe burn covering over 33% of his body.
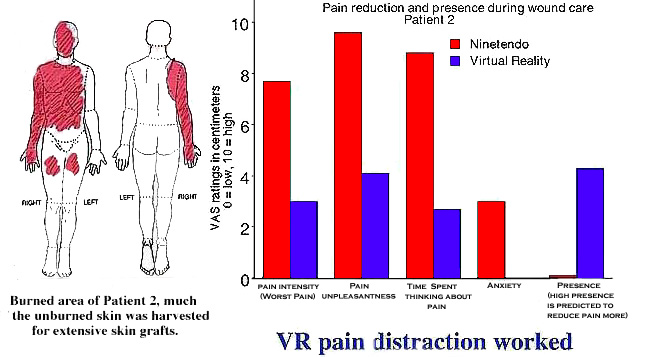
Patient 2 showed a similar large but less
extreme pattern (reduction of pain during wound care while in VR compared to
while playing a video game). The results of these two patients are described
in a clinical note in the March 10th, 2000 issue of the medical journal PAIN.
Clinical notes are inconclusive by nature, and larger studies are needed (and
underway).
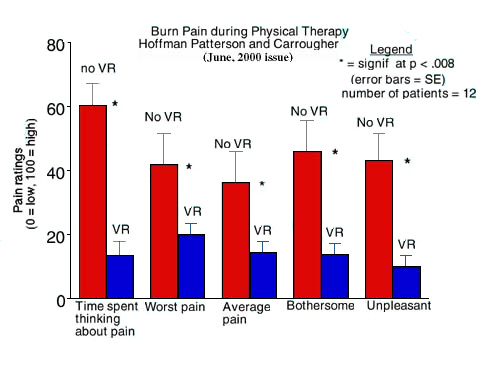
In a related preliminary clinical study
that is now completed, (Hoffman, Patterson and
Carrougher, 2000), have found additional support for the efficacy of VR
for pain control. Twelve patients with severe burns at Harborview reported
highly significant reductions in pain levels during physical therapy when in
VR compared to no VR (conventional treatment). In addition to distracting the
patients, VR can likely be used to motivate patients to perform desired
stretching motions, using behavioral reinforcement techniques (e.g., they
could get more gas for their jet by gripping and ungripping their healing
hand 10 times).
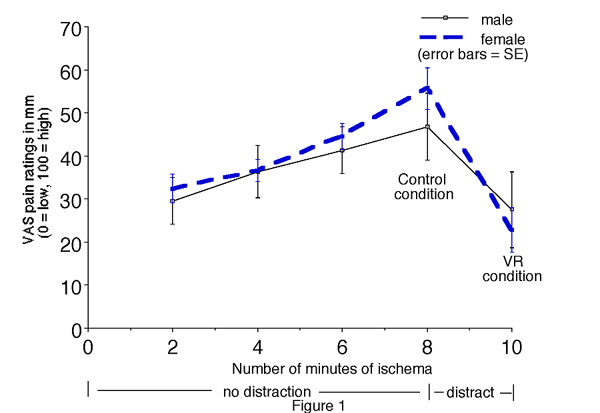
A controlled analog laboratory study using healthy volunteers has also shown
encouraging preliminary results.
As shown in the graph below, a
controlled analog laboratory pain study using healthy volunteers has also
shown encouraging results (Hoffman, Garcia-Palacios, Kapa, Beecher, &
Sharar, 2003). With no distraction, pain went up and up every two minutes, as
is typical of 10 min blood pressure cuff ischemas. During the last two
minutes, subjects went into virtual reality, and their pain dropped
dramatically.
In all of our VR pain control studies, patients, (especially children and
teenaged burn patients) have shown enthusiasm about participating.

Harborview occupational therapist Dana Nakamura stretching a young female
patient's healing skin during physical therapy,while the patient explores
SpiderWorld.
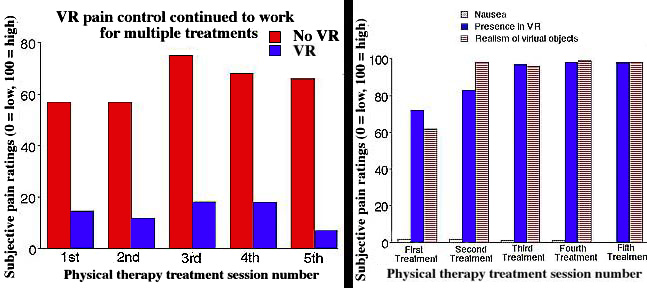
Use
of VR on multiple occassions with the same patient have been reported by Hoffman Patterson, Carrougher and Sharar, 2001;
and Hoffman Patterson, Carrougher, Nakamura et al.,
Additional
downloadable VR Research Papers.
Information
about CyberTherapy 2005: June 6-10, 2005, Basil, Switzerland
Publications
in scientific journals in 2000-2005.
Hoffman HG, Doctor JN, Patterson DR, Carrougher
GJ, and Furness TA III. Use of virtual reality for adjunctive treatment of
adolescent burn pain during wound care: A case report. Pain, 2000
85:305-309.
Thanks to the generosity of Elsevier
Publishing. A short version of this paper (not the full text) is available
for download (CLICK HERE TO
DOWNLOAD SMALL PAIN MANUSCRIPT).
The image above shows Verna Cain, RN,
treating our first burn patient during wound care with VR analgesia (VR is
used in addition to traditional opioids). Photo by Gretchen
Carrougher, RN, and female computer graphics artist wonder Miss Howard
Chambers (a talented young woman named Howard).
For the full text article please see http://www.elsevier.com
for reprint or subscription info.
Hunter Hoffman (August, 2004). Virtual Reality Therapy. Scientific American
Magazine. (Please also see www.sciam.com for subscriptions).
Hoffman HG, Richards T.L. Coda B, Bills,
AR, Blough D., Richards AL, Sharar SR. Modulation of thermal
pain-related brain activity with virtual reality: evidence from fMRI.
Neuroreport. 15(8):1245-1248, June 7, 2004.
Hoffman HG, Sharar SR, Coda B, Everett
JJ, Ciol M, Richards T, Patterson DR. Manipulating presence influences the
magnitude of virtual reality analgesia. Pain. 2004 Sep;111(1-2):162-8.
Hoffman HG, Patterson DR,
Magula J, Carrougher GJ, Zeltzer K, Dagadakis S, Sharar SR.
Water-friendly virtual reality pain control during wound care. J Clin
Psychol. 2004 Feb;60(2):189-95.
Hoffman, H.G., Garcia-Palacios, A., Kapa, V.A., Beecher, J. & Sharar,
S.R. (2003). Immersive Virtual Reality for reducing experimental ischemic
pain. International Journal of Human-Computer Interaction, 15, 469-486. (not
presently available for download).
Hoffman, H.G.,
Patterson, D.R., Carrougher, G.J. Use of virtual reality for adjunctive
treatment of adult burn pain during physical therapy: A controlled study. The
Clinical Journal of Pain. 2000 16:244-250.
Thanks to the generosity of Lippincott,
Williams and Wilkins, results from Hoffman, Patterson and Carrougher, 2000,
abstract, graphs and summary (but not full text) are available for download (CLICK HERE TO
DOWNLOAD SMALL "VR physical therapy" MANUSCRIPT),
Please see http://Lww.com for reprint or
subscription information to get the full article.
Hoffman, H.G.,
Patterson, D.R., Carrougher, G.J., and Sharar, S.R. The effectiveness of
virtual reality-based pain control with multiple treatments. The Clinical
Journal of Pain. 2001 17:229-235
Hoffman, H.G., Richards,
T., Coda, B., Richards, A., and Sharar, S.R. The illusion of presence in
immersive virtual reality during and fMRI brain scan. CyberPsychology
& Behavior. 2003 6(3):127-131.
PDF Version (308kb)
Please see CyberPsychology
& Behavior for reprint or subscription information.
Difede, J., Hoffman,
H.G. Virtual reality exposure therapy for World Trade Center post-traumatic
stress disorder: a case report. CyberPsychology & Behavior 2002
5(6):529-535.
PDF Version (149kb)
Please see CyberPsychology
& Behavior for reprint or subscription information. We have also
submitted several additional VR pain scientific papers for publication.
Please check back in a few months in case we have posted these additional
results for download (once they go through the review process and are
accepted for publication)!
Garcia-Palacios, A.,
Hoffman, H. G., Carlin, C., Furness, T.A. III, Botella-Arbona, (2002).
Virtual reality in the treatment of spider phobia: A controlled study.
Behaviour Research and Therapy, 40:9;983-993.
Hoffman HG, Richards TL, Magula J,
Seibel EJ, Hayes C, Mathis M, Sharar SR, Maravilla K. A
magnet-friendly virtual reality fiberoptic image delivery system.
Cyberpsychol Behav. 2003 Dec;6(6):645-8.
Steele E, Grimmer K, Thomas B, Mulley B,
Fulton I, Hoffman H.
Virtual reality as a pediatric pain modulation technique: a case study.
Cyberpsychol Behav. 2003 Dec;6(6):633-8.
To Contribute to expanding the use of
VR for pain control
Please write "for
VR Pain project" on the memo line of your check payable
to: Harborview
Medical Center and send it to:
Harborview Office of Development,
Box 359950,
University of Washington,
Seattle, 98104.
If you need a tax receipt (since these gifts are tax deductable), please
mention this important fact in a short letter.
If you have questions, please feel free to
call Harborview Office of Development at: (206) 521-1666
Thanks a lot!
Contacts
Dr. Hunter
Hoffman, hunter hitl.washington.edu hitl.washington.edu
|
















